From combat to operating room: The lifesaving potential of absorbable hemostats
 |
Uncontrollable bleeding is one of the leading causes of fatalities in military and hospital settings. In combat scenarios, up to 50% of deaths result from exsanguination, with 80% attributed to noncompressible injuries. In civilian emergencies, hemorrhage accounts for one-third of prehospital deaths, a statistic that remains largely unchanged over the decades. Additionally, surgeries like cardiovascular and orthopedic procedures often involve significant blood loss, creating critical challenges for patient safety [1].
Effective hemostasis — the process of stopping bleeding — is essential to improve surgical outcomes and save lives. In recent years, absorbable hemostats have emerged as an effective solution to manage bleeding. These tools reliably control bleeding without requiring removal, minimizing complications and supporting faster recovery.
This brings us to a key question: what exactly are absorbable hemostats?
What are Absorbable Hemostats?
Absorbable hemostats are medical devices used in surgery to control bleeding, especially when traditional methods like ligature or pressure are not enough.Unlike traditional agents, these hemostats are biodegradable and are naturally absorbed by the body over time. This eliminates the need for removal, making them especially useful for deep or hard-to-reach surgical sites.
How Do Absorbable Hemostats Work?
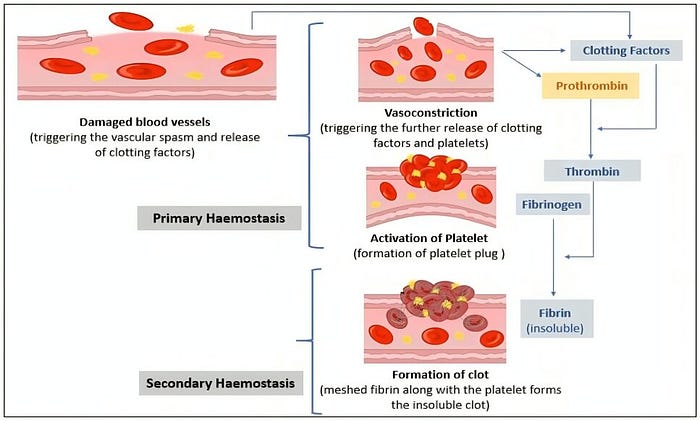
Absorbable hemostats function by supporting the body’s natural haemostatic processes. To understand their action, it’s essential to know the key steps of haemostasis [4]:
1. Vasoconstriction
When an injury occurs, the blood vessels narrow in a process called vasoconstriction. This initial response reduces blood flow to the affected area, minimizing blood loss.
2. Platelet Activation and Plug Formation
In the first stage of haemostasis, known as primary haemostasis, platelets are activated upon exposure to collagen at the injury site. These small blood cell fragments become sticky, adhering to the damaged vessel wall and to each other, forming a temporary platelet plug to seal the wound.
3. Coagulation Cascade and Fibrin Clot Formation
Secondary haemostasis, or the coagulation cascade, involves a series of reactions among clotting factors that stabilize the platelet plug. Fibrinogen is converted into fibrin, creating a mesh-like structure that reinforces the plug and traps red blood cells, forming a durable clot.
4. Clot Retraction and Stabilization
After the clot forms, it undergoes retraction, where it contracts and pulls the edges of the wound together. This process helps limit further bleeding and supports the healing of the injured vessel.
5. Fibrinolysis
Once the injury has healed, fibrinolysis begins to dissolve the fibrin clot. This ensures normal blood flow is restored and prevents excessive clot formation, completing the healing process.
Absorbable hemostats work in two primary ways to mimic or enhance these natural steps [5]:
I. Coagulation Activation
Some absorbable hemostats actively interact with blood components to accelerate clot formation.
- These agents stimulate the body’s natural coagulation cascade by engaging platelets and clotting factors at the site of bleeding.
- By promoting the rapid conversion of fibrinogen to fibrin, they facilitate the creation of a stable clot that effectively seals the wound.
- Such hemostats are classified as active agents due to their biological activity while directly participating in the coagulation process [6].
II. Barrier Formation
Other absorbable hemostats such as SURGISPON® and Surgi-ORC® function passively by providing a physical structure that promotes platelet aggregation and clot development.
- These devices act as a mechanical barrier, blocking blood flow at the site of injury.
- The structure serves as a scaffold, allowing platelets to adhere and aggregate, forming a protective clot.
- These are referred to as passive agents because they do not directly interact with the coagulation cascade but instead support the natural clotting process [7].
These agents are gradually absorbed by the body, making them ideal for surgeries where removal is impractical.
But what makes a hemostat truly effective? Let’s take a closer look.
Characteristics of an Ideal Absorbable Hemostat
When selecting an absorbable hemostat, the following attributes are important:
- Excellent flexibility for good handling
- Promptness and effectiveness in control/cessation of bleeding
- Ease of preparation
- Ability to make effective contact with the bleeding surface
- Stable absorption by the body
- Components that do not cause an immune response
- Trimming adaptability to fit the wound precisely
- Non-adherence to instruments for smooth surgical handling
- Antimicrobial effect against resistant microorganisms
- An acceptable adverse-event profile
- Availability in various sizes, shapes, and forms for different surgical needs
The outcomes of haemostatic agents vary depending on their specific characteristics [5, 8].
Surgical Application Areas

Absorbable hemostats are used across various surgeries, making them a versatile tool in modern healthcare.
Understanding their qualities helps explain why they’re so valuable in surgery.
Advantages of Absorbable Hemostats
Absorbable hemostats have transformed surgical practices due to their numerous advantages:
- No need for removal: Their biodegradable nature ensures they dissolve naturally, making them ideal for complex or deep surgical sites.
- Reduced risk of Infection: Leaving foreign materials in the body can increase infection risk, but absorbable hemostats reduce this concern by disappearing over time [9].
- Rapid action: Surgeons can quickly achieve hemostasis, allowing them to focus on other aspects of the procedure [10].
- Enhanced patient outcomes: With fewer complications, patients often experience faster recovery times and better overall results.
- High absorption capacity: Absorbs several times its own weight in fluid, making it effective for heavier bleeding.
And while they’re already making a difference, their future holds even more potential.
Future Trends and Innovations
The future of absorbable hemostats looks promising, with several exciting advancements on the horizon [11]:
- Development of advanced biomaterials
Research into advanced biomaterials, such as nanocomposites and bioengineered polymers, focuses on enhancing hemostatic efficacy by incorporating agents like tranexamic acid and platelet-rich fibrin (PRF), offering improved outcomes in diverse conditions, including coagulopathies and anticoagulant therapy [12].
- Minimizing adverse reactions
Efforts are focused on reducing immunogenicity, toxicity, and infection risks while maintaining high efficacy, particularly in sensitive applications like neurosurgery.
- Integration with regenerative therapies
Hemostats are combined with wound-healing agents, such as growth factors or stem cells, to accelerate tissue repair and improve long-term outcomes.
- Multifunctional hemostats
Hemostats are designed to incorporate antimicrobial, anti-inflammatory, and hemostatic properties, addressing multiple clinical needs simultaneously.
All of this points to one thing: absorbable hemostats are here to stay.
Conclusion
Absorbable hemostats are redefining bleeding management in surgical and emergency care by providing effective, natural, and reliable solutions. By reducing the risk of infection and eliminating the need for removal, these hemostats contribute to smoother recovery and promote safer surgical environments. Additionally, their ease of use and adaptability across various procedures enhance operational efficiency, allowing surgeons to focus on other critical aspects of patient care. With advancements in biomaterials and technology, absorbable hemostats are paving the way for more streamlined, patient-centered surgical practices.
Comments
Post a Comment